When the retina tears and pulls away from its normal position at the back of the eye, the retina is considered to be “detached.†Once pulled away, the retina no longer works properly and loses its blood supply. Retinal tears and detachments are serious problems that result in blindness unless treated.
https://www.youtube.com/watch?v=pPQr6BgzhDA
https://www.youtube.com/watch?v=z-5jgIdohog
The retina is the nerve layer at the back of the eye that senses light and sends images to your brain. Like a camera, the lens in the front part of the eye focuses light onto the retina. The retina is like the film that lines the back of the camera and is where the image is captured.
When the retina is pulled away from its normal position at the back of the eye, the retina is considered to be “detached.†Once pulled away, the retina no longer works properly and loses its blood supply. A retinal detachment is a very serious condition that results in blindness unless treated.
Causes of retinal tears and retinal detachment:
Except in the case of blunt trauma to the eye itself, the development of retinal tears and detachment is not related to activity, diet or any other factor in daily life. There is a genetic predisposition to retinal tears and detachment as they frequently run in families.
Posterior Vitreous detachment:
The middle of the eye is filled with a clear gel called the vitreous. As we age, the vitreous can pull away from its attachment to the retina at the back of the eye. This is called a posterior vitreous detachment. You may notice flashes and/or floaters in your vision. The flashes represent the vitreous gel pulling on the retina. The floaters represent the remnants of the vitreous gel floating through the cavity of your eye, or sometimes blood. Everyone eventually develops a posterior vitreous detachment. In most cases, the vitreous separates from the retina cleanly without a problem, and in most cases the flashes and floaters slowly resolve over time. You can maintain your normal activity level.
Retinal Tears:
In some cases, there is an abnormally tight adhesion between the retina and the vitreous. When the vitreous pulls away it can create a tear in the retina. Only a small minority of people will develop retinal tears when the gel pulls away. Unfortunately, there are no specific symptoms indicating you may have a retinal tear. Anyone with the onset of flashes or floaters could be having a vitreous detachment and thus may develop a tear. They should be seen within 24-72 hours for a dilated fundus exam to check for the development of retinal tears. Retinal tears are most easily treated in an office setting with laser photocoagulation. This treatment prevents the retinal tear from becoming a more serious retinal detachment.
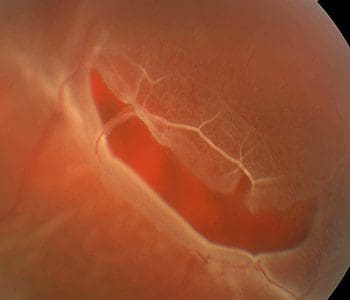
Retinal Detachment:
If retinal tears are not found and treated promptly, fluid can pass through these tears lifting the retina off the back of the eye and causing a retinal detachment.
Warning Symptoms of Retinal Detachment:
These symptoms may indicate that a retinal detachment has occurred:
- Flashes and/or new floaters followed (days to weeks later) by:
- A shadow in your peripheral field of vision
- A grey curtain moving across you field of vision
While these symptoms do not always mean a retinal detachment has occurred, the doctor can help diagnose this condition during an eye examination by dilating the pupils of your eyes.
The following conditions may increase your chance of having a retinal detachment:
- Nearsightedness
- Prior cataract surgery
- Severe injury or trauma
- Previous retinal detachment in your other eye
- Family history of retinal detachment
- Weakened areas of your retina that can be seen and diagnosed by Dr. Comaratta
Treatment of Retinal Tears:
The doctor treats retinal tears with laser surgery performed in the office. The goal of treatment is to “spot-weld†the tears and to seal the retina to the back wall of the eye. This prevents fluid from passing thru the tear and causing a retinal detachment. There is usually very little discomfort following the procedure. Patients are encouraged to return to normal activity immediately. They are cautioned to monitor their vision for the onset of new floaters and/or flashes which could indicate the onset of new retinal tears. The development of a shadow or curtain could indicate a retinal detachment.
Treatment of Retinal Detachment:
The doctor treats retinal detachments by surgically returning the retina to its proper position. The doctor has great expertise in determining which surgical method is right for each patient. He routinely performs the following repair procedures:
Pneumatic Retinopexy
This procedure is performed in the office. The doctor injects a gas bubble into the vitreous space inside the eye. The gas bubble pushes the retinal tear closed against the back wall of the eye. This procedure requires that the patient maintain a certain head position for several days depending upon the position of the retinal tear(s). Once the retina is reattached, the doctor will perform laser treatment to seal the retinal tears permanently. The gas bubble gradually dissipates over the course of several weeks. This procedure allows for a rapid recovery for the patient. Most can return to normal activity in 1-2 weeks. Unfortunately, not all patients are candidates for this procedure.
Scleral Buckle/Cryopexy
This is a procedure performed in the hospital operating room under local anesthesia with light sedation.This treatment involves identifying the retinal breaks and freezing them with a technique called cryopexy which creates an adhesion around the retinal tears, thereby sealing them. A soft silicone band called a scleral buckle is then placed around the eye, under the retinal tears to help close them and to counteract the force pulling the retina out of place. Occasionally, the doctor will drain the fluid beneath the detached retina to allow it to return to its normal position against the back wall of the eye. This procedure is more invasive with a recovery period of 4-6 weeks.
Scleral Buckle/Vitrectomy
The doctor typically uses this procedure to fix retinal detachments not amenable to pneumatic retinopexy. It is performed in the hospital operating room under local anesthesia with light sedation. It is a two step procedure. A scleral buckle is placed around the eye, under the retinal tears, to help close them and counteract the force pulling the retina out of place. A vitrectomy is then performed to remove the vitreous gel pulling on the retinal tears. The fluid underneath the retina is drained, the retinal tears are lasered, and a gas bubble is injected into the eye. The gas bubble helps to keep the retina in place until the laser treatment solidifies. The body’s fluids gradually replace the gas bubble over several days to weeks. The doctor may require you to maintain special head positioning for several days to a week after the surgery depending upon the nature of your detachment. The recovery period is generally 2-4 weeks.
After Surgery:
You can expect some discomfort after the completion of your procedure. Rarely will patients require more than Tylenol or ibuprofen to ease their discomfort.
